細胞培養進口血清進口胎牛血清進口新生牛血清進口豬血清馬血清
細胞培養進口血清進口胎牛血清進口新生牛血清進口豬血清馬血清 支原體檢測盒及標準品常規PCR檢測試劑盒熒光定量PCR檢測(qPCR法)支原體DNA提取靈敏度標準品(方法驗證用)特異性標準品(方法驗證用)PCR定量標準品(可用于方法驗證)
支原體檢測盒及標準品常規PCR檢測試劑盒熒光定量PCR檢測(qPCR法)支原體DNA提取靈敏度標準品(方法驗證用)特異性標準品(方法驗證用)PCR定量標準品(可用于方法驗證) 支原體祛除試劑細胞中支原體祛除環境支原體祛除水槽支原體祛除
支原體祛除試劑細胞中支原體祛除環境支原體祛除水槽支原體祛除 干細胞培養基
干細胞培養基 DNA/RNA污染祛除DNA/RNA污染祛除試劑DNA污染監測
DNA/RNA污染祛除DNA/RNA污染祛除試劑DNA污染監測 RNA病毒研究試劑RNA病毒檢測試劑盒病毒RNA提取
RNA病毒研究試劑RNA病毒檢測試劑盒病毒RNA提取 PCR儀器及配套產品DNA污染監測祛除PCR/qPCR儀性能檢查PCR試劑PCR試劑盒PCR預混液(凍干粉)熱啟動聚合酶MB Taq DNA
PCR儀器及配套產品DNA污染監測祛除PCR/qPCR儀性能檢查PCR試劑PCR試劑盒PCR預混液(凍干粉)熱啟動聚合酶MB Taq DNA 微生物PCR檢測食品檢測類產品食品微生物檢測細菌PCR檢測
微生物PCR檢測食品檢測類產品食品微生物檢測細菌PCR檢測
- 細胞培養進口血清進口胎牛血清進口新生牛血清進口豬血清馬血清
- 支原體檢測盒及標準品常規PCR檢測試劑盒熒光定量PCR檢測(qPCR法)支原體DNA提取靈敏度標準品(方法驗證用)特異性標準品(方法驗證用)PCR定量標準品(可用于方法驗證)
- 支原體祛除試劑細胞中支原體祛除環境支原體祛除水槽支原體祛除
- 干細胞培養基
- DNA/RNA污染祛除DNA/RNA污染祛除試劑DNA污染監測
- RNA病毒研究試劑RNA病毒檢測試劑盒病毒RNA提取
- PCR儀器及配套產品DNA污染監測祛除PCR/qPCR儀性能檢查PCR試劑PCR試劑盒PCR預混液(凍干粉)熱啟動聚合酶MB Taq DNA
- 微生物PCR檢測食品檢測類產品食品微生物檢測細菌PCR檢測
|
|
污染細胞的支原體從哪里來2016-09-23 13:40
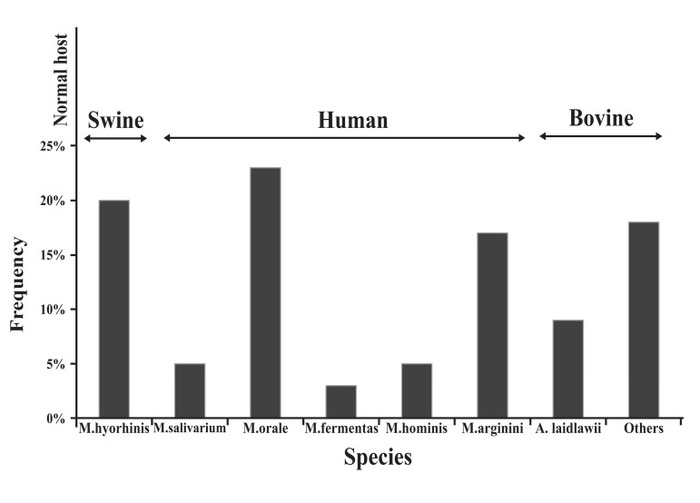
締一生物導讀: 在培養細胞時,人們常常關注細菌和真菌的污染,認為它們是細胞培養的主要干擾因素。但其實,更嚴重的是支原體 的感染,它的發生率非常高,而且不易被發現。不僅普通光鏡下無法發現支原體,而且培養基也不容易變色。但支原體對細胞的各種干擾卻是不容忽視的。它不僅導致細胞狀態不佳,生長速度慢,而且會使細胞內DNA、RNA及蛋白表達發生改變,嚴重影響實驗結果。因此,在預防和治療支原體污染之前,有必要去了解細胞被支原體污染的可能途徑。 支原體污染細胞的途徑(點擊這里,詳細了解支原體污染防治類試劑) 支原體可以通過頂部的細胞器特異性和宿主細胞結合。這些頂部的細胞器含有高濃度的粘附蛋白,可粘附到真核細胞并穿入到細胞內部。支原體缺乏細胞壁,它們的胞膜可和宿主的細胞膜融合并交換其胞膜和胞漿成分。 支原體污染的頻率和污染來源 細胞培養中有幾種支原體污染與人、牛和豬有關。實驗室的工作人員是口腔支原體、發酵支原體和人型支原體的主要來源。這三種支原體占細胞培養中支原體污染的一半以上,它們主要存在于人的口咽部。精氨酸支原體和無膽甾原體是另兩類細胞培養中的支原體,它們來自胎牛血清和新生牛血清。胰酶如果是豬來源的,那么也可能存在豬鼻支原體。圖1顯示了支原體的常見宿主以及污染細胞的發生率。
圖1:在細胞培養中出現的不同種類的支原體頻率 支原體在實驗室內的擴散來源 McGarrity設計了一個模型,來發現支原體是如何在超凈臺里的細胞傳代過程中發生傳播的。他先故意用支原體感染細胞。在超凈臺中,用胰蛋白酶消化該污染的細胞后發現,活的支原體可從細胞培養瓶外的細胞計數板、移液器、廢棄盤中被技術員分離出來。即使過了四至六天,活的支原體仍然可以存在于超凈臺表面,可被成功恢復。在超凈臺里,傳代完被支原體污染的細胞后,再傳代干凈的不含支原體的細胞,結果仍然在6周后被檢測出支原體陽性。這些結果表明,支原體的傳播是多么的快速和容易!它也警告我們,要**限度的避免支原體的污染,因為一瓶細胞發生污染,就會帶來支原體傳播的可能。 未真正消毒的耗材、培養基和溶液 不恰當的消毒導致污染的另一個原因。高壓鍋或干熱烤箱中堆積太多的物品造成加熱不均,使一小部分耗材未得到消毒。滅菌循環時間過短是另一個消毒上犯的錯誤,特別是對于超過500ml的液體,或者是包含固體成分的溶液,或膠體物質如瓊脂、淀粉等。為了實現無菌,滅菌材料的尺寸、質量、性質和體積必須始終考慮。 在無菌和無昆蟲區域存放消毒好的物品,使防止再次污染的前提。良好的無菌操作也是至關重要的。 實驗室人員 在因人導致的細胞支原體污染中,口腔支原體發生率最高,它主要存在人的口咽部。發酵支原體和唾液支原體也在污染的細胞培養液中被檢測出來,不過發生率更低。 被支原體污染的細胞 實驗室內細胞支原體的相互傳染,有必要對于從外源獲得的新的細胞系進行支原體檢測。一瓶細胞中的單個支原體的存在足以威脅到其他培養的細胞。支原體的污染能通過細胞操作產生的氣溶膠或液滴傳播。所以,應一次只操作一種細胞,為每種細胞系配置單獨的培養基和試劑,這能避免支原體的污染。 細胞培養的正確操作和對新培養的細胞定期檢查,可以減少支原體污染的機會。 威正翔禹生物原裝進口Ausbian特級胎牛血清,內毒素低,品質高,為您預留庫存,同批號跟蹤實驗數據更穩定,血清全程無凍融,讓細胞表現更出色!另外還有各種支原體檢測祛除試劑、細胞培養基、微生物培養基等,威正翔禹生物,為您科研室物料提供有力保障! 英文原文: Ways in which cells are contaminated by mycoplasma Mycoplasmas can bind to their host cells using special tip organelles. These tip organelles have a high concentration of adhesins, to attach to eukaryotic cells and penetrate the host cell. The lack of a stiff wall in mycoplasma may help it to fuse with the membrane of the host cell and exchange its membrane and cytoplasmic components. Frequency and sources of mycoplasma species There are a number of different sources for mycoplasma contamination in cell cultures associated with human, bovine and swine species. Personnel in the laboratories are the main sources of M. orale, M. fermentans, and M. hominis. These species of mycoplasmas account for more than half of all mycoplasma infections in cell cultures and physiologically are found in the human oropharyngeal tract . M. arginini and A. laidlawii are two other mycoplasmas contaminating cell cultures and originate in fetal bovine serum (FBS) or newborn bovine serum (NBS)。 Trypsin solutions provided by swines are a major source of M. hyorhinis. Figure 1 is a diagram showing the normal host and frequency of different species of mycoplasma occurring in cell culture. Different sources for the spreading of mycoplasma in the laboratory McGarrity designed a model to find out how mycoplasmas spread in a laminar flow hood during a routine subculturing procedure. He intentionally infected a cell culture with mycoplasma. After trypsinization of the infected culture in a laminar flow hood, live mycoplasmas were isolated by the technician, outside of the flask, a hemocytometer, the pipettor, and outside of the pipette discard pan. Live mycoplasma could be successfully recovered from the surface of the laminar flow hood even four to six days later! A clean culture, that was subcultured once a week in the same hood following the work with the contaminated cells, tested positive for mycoplasma after only 6 weeks. These results show how quickly and easily mycoplasma can spread and also warn us against the possibility of contamination of most if not all of the other cultures after the entry of a single mycoplasma infected culture into the laboratory. Nonsterile supplies, media and solutions Improper sterilization is a major source of biological contaminants. Packing too much into an autoclave or dry heat oven will cause uneven heating, resulting in pockets of nonsterile supplies. Using too short a sterilization cycle, especially for autoclaving volumes of liquids greater than 500 ml per vessel or solutions containing solids or viscous materials such as agar or starches are other mistakes resulting in incorrect sterilization. To accomplish sterility, the size, mass, nature and volume of the materials for sterilization have to always be considered . Storing sterilized supplies and solutions in a dust- and insect-free area is an obligation to prevent recontamination. Good aseptic technique is also crucial Laboratory personnel Laboratory personnel are considered a major source of mycoplasma contamination . Table 1 shows potential sources of cell culture contamination. M. orale, a species commonly found colonizing the human oral cavity and oropharynx, has been the leading contaminant in study after study. Two other human mycoplasma species, M. fermentans and M. salivarium, are also detected in contaminated cultures but at a much lower rate. Table 2 shows major mycoplasma species found in cell culture and also some of the research results reporting the percentage of contamination with different types of mycoplasma in previous years . Table 1: Potential sources of cell culture contamination. Other mycoplasma contaminated cell cultures A mycoplasma-infected cell culture is a major source of mycoplasma contamination of other cell cultures in the lab. To avoid mycoplasma contamination in cell cultures, it is recommended to test the new cell lines which are obtained from an outside source. A single mycoplasma contaminated cell culture is enough to endanger other cell cultures in the lab. The contamination can spread by means of aerosols and particulates generated during the handling of the mycoplasma infected cell culture. So, working with only one cell culture at a time and preparing separate media and reagents for each individual cell line can avert mycoplasma contamination . A good cell culture practice and regular testing of all new cell cultures can decrease the risk of mycoplasma contamination . 文獻出處:N Laleh,F Parvaneh. Prevention and Detection of Mycoplasma Contamination in Cell Culture. Cell Journal, 2012, 13(4): 203 版權聲明:版權歸原作者所有,如有版權問題,請與我們聯系。
|
 細胞培養進口血清
細胞培養進口血清 支原體祛除試劑
支原體祛除試劑 干細胞培養基
干細胞培養基